
Beyond Echo Chambers: Building a Balanced Neurodiversity‑Affirming Movement
DISCLAIMER: I write this from a perspective shaped by both privilege and adversity. I’ve benefited from access to education and hold a professional title that

DISCLAIMER: I write this from a perspective shaped by both privilege and adversity. I’ve benefited from access to education and hold a professional title that

I couldn’t scream. Yet, there were those inside that wished they did. A little girl who wanted to scream But instead was still. Frozen with
A program called Open to Debate recently invited me to debate the topic of whether or not Alcoholics Anonymous (AA), as a program of recovery,
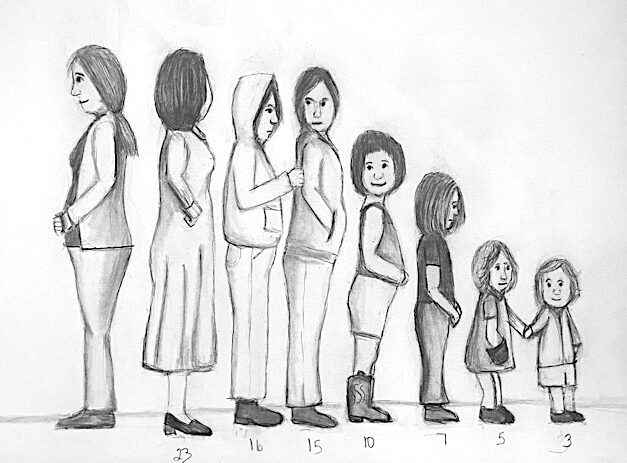
(CONTENT WARNING: This contains personal recollections of childhood sexual abuse, fat shaming, and eating disorders.) A few years ago, I decided it was time for
In a spiritual abuse course that I taught last week online, many survivors poured out their hearts and souls about how much their respective churches

I Will Rise was performed at the closing ceremony of the Redefine Therapy Expressive Arts Retreat April 28th, 2024. Judy and Alicia worked together, in the moment, to bring movement and dance into Judy’s poem in a call and response collaboration.

Dr. Jamie Marich explores their journey through addiction recovery and trauma treatment, emphasizing the transformative power of honesty in confronting societal stigmas, challenging clinical norms, and advocating for authenticity and inclusivity in trauma care.

“Girl, I heard you speak for 10 minutes and I knew they couldn’t keep you locked up in the university.” This comment, delivered with enthusiasm

To dance is my rebellion. To move this body through time and space, to move unapologetically, expansively, refusing to shrink, to be silent, to disappear.